Osteoarthritis is one of the most common musculoskeletal diseases globally, especially among middle-aged and older adults. This condition not only causes persistent pain but also impairs motor function, severely affecting daily quality of life. However, this is a completely manageable and improvable condition if diagnosed early and treated with the right methods, especially physical therapy.
This article, with consultation from experts at MBJ Clinic, will provide a comprehensive overview of osteoarthritis – from its definition, causes, and warning signs to the most advanced and effective treatment methods available today.
Nội dung
- 1 I. What is Osteoarthritis?
- 2 II. Common Causes of Osteoarthritis
- 3 III. Early Signs and Symptoms of Osteoarthritis
- 4 IV. The Four Stages of Osteoarthritis Progression
- 5 V. The Most Common Joints Affected by Osteoarthritis
- 6 VI. Current Diagnostic Methods for Osteoarthritis
- 7 VII. Effective Treatment Methods for Osteoarthritis
- 8 IX. Frequently Asked Questions (FAQ)
I. What is Osteoarthritis?
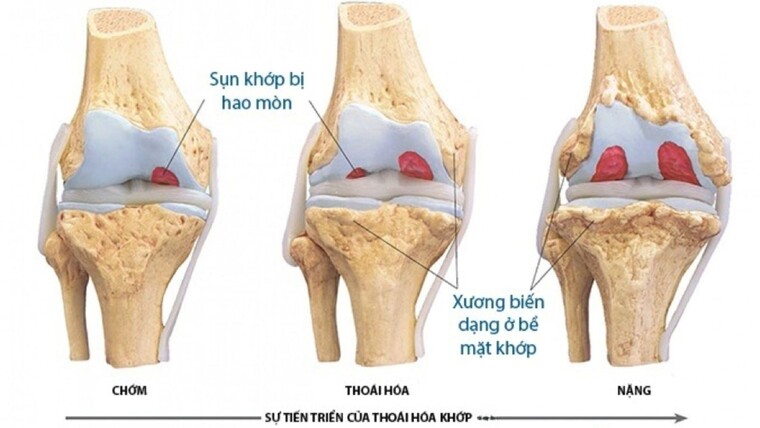
Scientifically and simply put, Osteoarthritis is a condition involving the damage and erosion of articular cartilage (the cushioning layer covering the ends of bones) and the subchondral bone beneath it.
The disease mechanism begins when the cartilage layer, which acts as a shock absorber, wears down over time or due to external factors. When the cartilage is damaged, the bone ends can rub directly against each other during movement, causing pain, swelling, and stiffness. Concurrently, the body initiates an inflammatory response, forming bone spurs and reducing synovial fluid, making movement even more difficult.
II. Common Causes of Osteoarthritis
Osteoarthritis is divided into two main causal groups:
Primary Causes: This is the natural aging process of the body. Age is the leading risk factor. As people get older, the quality of their cartilage declines, making it more susceptible to wear and tear.
Secondary Causes: These include external factors or other medical conditions:
- Injuries and Accidents: Joint injuries such as fractures, sprains, meniscal tears, or ligament damage can accelerate the degenerative process.
- Overweight and Obesity: Excess body weight increases pressure on weight-bearing joints like the hips, knees, and spine, causing cartilage to wear down faster.
- Genetics: Some individuals have a genetic predisposition that makes their cartilage weaker and more prone to early degeneration.
- Congenital Joint Deformities: Abnormalities in joint structure from birth can cause uneven force distribution, leading to osteoarthritis.
- Metabolic Diseases: Conditions like diabetes, gout, or endocrine disorders can affect cartilage health.
- Lifestyle and Work Habits: Prolonged sitting or standing in poor posture, frequently carrying heavy loads, and a sedentary lifestyle are all factors that promote the disease’s progression.
III. Early Signs and Symptoms of Osteoarthritis
The symptoms of osteoarthritis usually develop slowly and worsen over time. Early recognition of the following signs is crucial:
- Joint Pain: This is the most typical symptom. The pain often increases with activity and subsides with rest. In advanced stages, the pain may be constant.
- Morning Stiffness: Patients often feel that their joints are stiff and difficult to move after waking up, a condition that typically lasts for about 15-30 minutes.
- Crepitus (Grating or Crackling Sound): This sound occurs when the unsmooth bone ends rub against each other due to the loss of cartilage.
- Swelling, Warmth, and Redness: These are signs of an inflammatory response as the disease progresses.
- Reduced Range of Motion: Patients have difficulty performing movements such as bending, extending, or rotating the joint. For example, difficulty bending over, squatting, or turning the neck.
IV. The Four Stages of Osteoarthritis Progression
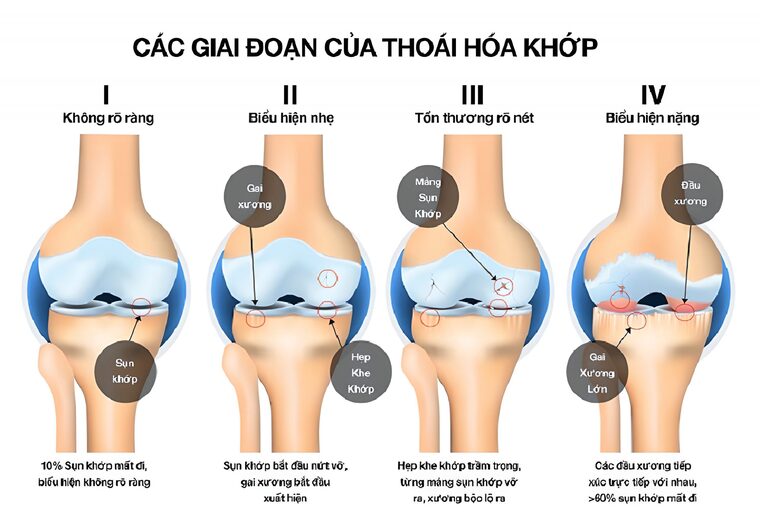
Osteoarthritis is a disease that progresses over time. Understanding each stage helps patients achieve early recognition and timely intervention. The disease typically goes through four main stages:
1. Stage 1: Initial Stage (Very Mild)
- At this stage, cartilage damage is minimal, around 5% – 10%.
- The patient experiences almost no symptoms or only very mild, transient pain during strenuous activity.
- Daily activities proceed normally.
- The condition is often not clearly visible on X-ray images at this stage.
2. Stage 2: Mild Stage
- X-rays may show a slight narrowing of the joint space and the formation of small bone spurs.
- The patient experiences more noticeable pain during continuous or heavy activity.
- Some may experience stiffness after waking up or aching when the weather changes.
3. Stage 3: Moderate Stage (Severe)
- Symptoms are now pronounced, with pain occurring frequently even during simple activities like walking or climbing stairs.
- The cartilage layer is severely damaged, the subchondral bone is deformed, and more bone spurs have formed.
- Without intervention, the cartilage can break down, causing an inflammatory reaction and joint effusion (also known as synovitis), leading to redness and swelling.
4. Stage 4: Very Severe Stage
- This is the most severe stage, with damage clearly visible on X-rays.
- The joint space is severely narrowed, and large bone spurs cause intense pain even at rest.
- The bone ends may be completely worn down and deformed, and a sharp decline in synovial fluid makes movement extremely difficult, potentially leading to disability.
V. The Most Common Joints Affected by Osteoarthritis
Osteoarthritis can occur in any joint but is most common in the following locations:
- Spinal Osteoarthritis:
- Cervical Osteoarthritis (Neck): Causes pain and stiffness in the neck and shoulder area, with pain that can radiate down the arm, causing numbness in the hands and muscle weakness.
- Lumbar Osteoarthritis (Lower Back): Causes a dull or sharp ache in the lower back, with pain that can radiate down the buttocks and legs (sciatica).
- Hip Osteoarthritis: Causes pain in the groin and front of the thigh, which may radiate to the knee. Patients have difficulty walking, standing up, or spreading their legs.
- Knee Osteoarthritis: Very common, causing pain especially when going up and down stairs, standing for long periods, or walking. The knee may become swollen and deformed (bow-legged).
- Hand Osteoarthritis: Causes pain, swelling, and the formation of small bony lumps on the finger joints, reducing grip strength.
VI. Current Diagnostic Methods for Osteoarthritis
To accurately diagnose osteoarthritis, a doctor will combine:
Clinical Examination: The doctor will ask about medical history and symptoms, check the range of motion, and look for points of pain, swelling, and other abnormalities in the joint.
Imaging Diagnostics:
- X-ray: The most common method, used to detect signs like joint space narrowing, bone spurs, and subchondral bone sclerosis.
- Magnetic Resonance Imaging (MRI): Provides detailed images of cartilage, ligaments, tendons, and other soft tissues to comprehensively assess the extent of damage.
- CT Scan: Used less frequently but may be necessary in some complex cases.
VII. Effective Treatment Methods for Osteoarthritis
The goals of osteoarthritis treatment are to relieve pain, improve motor function, slow the progression of the disease, and enhance the patient’s quality of life.
1. American-Standard Conservative Treatment at MBJ: No Drugs – No Surgery
At MBJ Clinic, we pioneer an American-standard treatment protocol for osteoarthritis, designed by a council of Musculoskeletal specialists based on the “3 No’s” standard: No drugs, no injections, no surgery. With experience in successfully treating thousands of patients, MBJ is proud to be a reputable provider of a safe, effective, and root-cause solution.
Our protocol is a close combination of manual therapy and high technology:
- Intensive Manual Physical Therapy A specialist doctor and a team of therapists directly perform physical techniques on the patient’s tense muscle areas. These manipulations soften and relax spastic muscles, stimulate blood circulation, and create a solid foundation for high-tech therapies to be maximally effective.
- Leading Treatment Technology from the US and Europe MBJ Clinic is proud to be the leading unit in Musculoskeletal treatment technology in Binh Duong. Our entire system of machinery is imported from the US and European countries and is certified by the US FDA for safety.
- Tecar Therapy – Super Pain Relief Technology: This FDA-approved technology uses a high-frequency current to transfer energy deep into damaged bone tissue, providing instant pain relief after just the first 20-minute session. This method stimulates the body’s self-healing process with up to 98% efficiency.
- High-Intensity Laser Therapy: The fourth-generation laser, with the widest wavelength and strongest intensity available today, can stimulate deep into bone tissue, helping to regenerate cells, promote healing, and effectively reduce swelling and inflammation.
- Chattanooga Multi-Frequency Ultrasound: This technology, 100% transferred from the US, combines ultrasound and heat therapy to eliminate pain instantly after 20 minutes. This therapy helps relax stiff muscles and joints, deeply reduces swelling and inflammation, and provides comfort to the patient.
- Rehabilitation Exercises At the end of each session, patients are guided through customized rehabilitation exercises. These exercises help strengthen muscles, maintain maximum treatment results, and, most importantly, establish correct movement habits to prevent recurrence.

2. Medical Treatment (Using Medication)
The use of medication requires a prescription and close monitoring by a specialist.
- Pain Relievers and Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) or Paracetamol.
- Muscle Relaxants: Used when muscle spasms are present.
- Intra-articular Injections: Injections of Corticosteroids or Hyaluronic Acid (an artificial lubricant) directly into the joint for rapid pain and inflammation relief.
3. Surgical Intervention
Surgery is only considered when conservative treatments are no longer effective and the disease is in an advanced stage, severely impacting life.
- Types of Surgery: Arthroscopic debridement (joint cleaning), osteotomy (bone realignment), or arthroplasty (joint replacement), most commonly for the hip and knee.
VIII. Home Care and Prevention of Osteoarthritis
“Prevention is better than cure.” Proactively caring for your joint health can effectively slow the degenerative process.
- Scientific Diet: Supplement with foods rich in Calcium, Vitamin D, Omega-3s (found in fatty fish, nuts), and antioxidants (green vegetables, fruits). Limit processed foods, sugar, and saturated fats.
- Weight Management: Maintaining a healthy weight is the best way to reduce pressure on the knees, hips, and spine.
- Appropriate Exercise: Opt for low-impact sports like swimming, cycling, yoga, or Tai Chi.
- Avoid Poor Posture: Keep your back straight when sitting and standing, and avoid squatting, deep knee bends, or carrying excessively heavy loads.
IX. Frequently Asked Questions (FAQ)
1. Can osteoarthritis be completely cured?
Osteoarthritis is a natural aging process and cannot be “cured” in the sense of reversing the damage. However, modern treatments, especially physical therapy, can effectively control symptoms, slow the disease’s progression, restore motor function, and help you lead a nearly normal life.
2. What should I eat and avoid if I have osteoarthritis?
- Should eat: Calcium-rich foods (milk, cheese), omega-3s (salmon, herring), vitamins C and K (green vegetables, fruits), Glucosamine, and Chondroitin (bone broth).
- Should avoid: Greasy foods, fast food, red meat, organ meats, sugary foods, and stimulants like alcohol and beer.
3. Is the cost of treating osteoarthritis high?
The cost of treatment depends on many factors, such as the severity of the disease, the chosen treatment method, and the individual’s treatment course. At MBJ Clinic, we will provide a clear and transparent treatment plan and cost estimate after an initial examination to ensure the most effective and suitable path for you.
Conclusion
Osteoarthritis is a challenge, but it is not the end of an active and joyful life. Early diagnosis and choosing the right treatment method, especially conservative approaches like Physical Therapy and Rehabilitation, are the golden keys to controlling pain and maintaining mobility.
Don’t let the pain of osteoarthritis affect your life. Contact MBJ Rehabilitation Specialty Clinic today to be consulted by leading experts and to have a customized treatment plan developed for you.

 Tiếng Việt
Tiếng Việt

